There’s a lot of observations that people with restrictive food disorder Anorexia Nervosa notice that others may not.
Not only are they analysing and calculating every piece of food they consume, every step they take and every gram they see on the scales.
People with this eating disorder are also calculating where they eat, how they eat, who is or isn’t in the room when they eat.
It is all a delicate, calculated and conscious balancing act to preserve their sense of identity – either within the disease or in the fight against it.
It’s an all-consuming and ever-present disorder.

What those with the disorder may not consider, however, is the impact their gut health is having on their physical and mental wellbeing, not to mention their rehabilitation efforts to combat the country’s deadliest mental heath disorder.
This is a consideration Deakin University PhD student Madeline West and her supervisor Dr Tetyana Rocks want to focus on.
They aim to shine a light on the gut microbiota of patients with anorexia in a world-first study, titled The Recovering Gut Study.
The team behind the study
West is a nutritionist and PhD student within the Food & Mood Centre, part of the Deakin University Innovation in Mental and Physical Health and Clinical Treatment strategic research centre (IMPACT).
Dr Rocks is also a member of the Food & Mood Centre, and an accredited practicing dietitian who has completed a PhD in eating disorders.
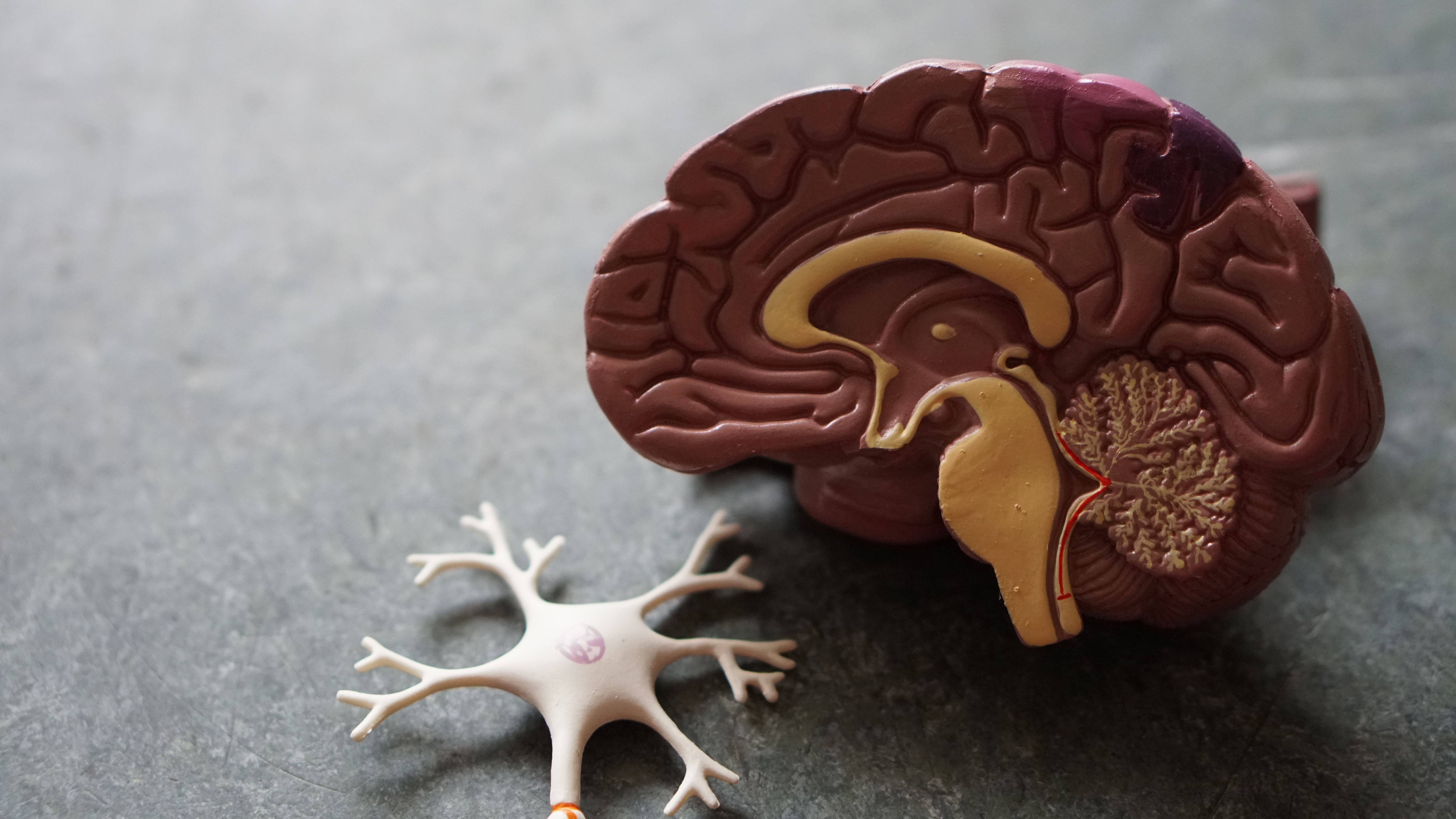
“We see gut microbiota composition and function affecting many aspects of human health and disease.
“We see gut microbiota impact in weight, metabolic outcomes, appetite, behaviour, food preferences and we know that all of these factors are usually disrupted in anorexia nervosa,” says Dr Rocks.
What is Anorexia Nervosa?
Anorexia Nervosa (AN) is defined as a psychiatric condition, characterised by low body weight due to restricted energy intake, coupled with a fear of gaining weight and a distorted body image.
While it is prevalent in approximately 1-2% of the general population of Australia, AN has the highest death rate of all psychiatric disorders.
In 50-97% of cases, AN is paired with other co-morbid psychiatric conditions such as depression and anxiety disorders.
“The success rate is only about 50%,” says Dr Rocks, “and it’s notoriously difficult for individuals who have an eating disorder (particularly AN – a restrictive eating disorder) to gain weight.”
The Recovering Gut Study is an observational study that aims to tackle the treatment and reha-bilitation outcomes of individuals with AN by analysing the gut microbiota composition and function.
The study will look at patients undergoing treatment in a 40-day private clinic.
Hoping to begin recruiting patients from early in 2020, the study will involve 40 participants diagnosed with either AN or a-typical AN.
Researchers will connect with patients once they’re admitted to the clinic, collecting faecal samples – which is how the gut microbiota is analysed – as well as a detailed questionnaire.
This questionnaire covers their physical activities; food choices and behaviours; gastrointestinal symptoms (such as bloat-ing, distention or constipation); and mental wellbeing (including mood, anxiety and depression).
They will then collect the same data at the end of treatment, and again 80 days after they have left the clinic.
West and Dr Rocks want to explore the impact the rehabilitation process has on the gut microbiota of AN patients, which often involves the re-introduction of foods previously restricted by those with AN.
“Considering the role that we know diet plays around gut microbiota, it’s fairly logical to assume there would be a difference in the patients who are severely restricting their eating, so that’s why we’re specifically interested in what’s happening after that process of re-introducing foods and what effect that’s going to have on what’s going on in their gut,” says West.
The gut-brain axis
The impact gut health has on physical and mental wellbeing is a relatively new area of research that is only now being explored.
Known as gut-brain axis, the bi-directional communication between the gut and the brain has shown direct and indirect pathways between gut microbiota and cognitive and emotional centres in the brain.
Advances in analytical technology and methods have made research into the gut-brain axis more accessible in recent years, though using the latest methods does come with a cost.
“It is a new area of research but we have a good collaborative relationship with a very advanced analytical companies and also very generous support from our philanthropical organisations, such as the Wilson Foundation and the Fernwood Foundation, who support Food & Mood and the research we’re doing,” says Dr Rocks.
“We will have the latest technology, the latest analytical methods using genomic sequencing in our study, which is going to be exciting,” adds West.
By exploring this new area of gut research, the team hope to not only find a link between gut mi-crobiota and the factors that may cause AN.
They are also looking to investigate how gut micro-biota composition may play a role in recovery from the disorder – such as why some people can recover and some people can’t.
“In the long term, one of the things that I’m really interested in is whether we can come up with improved nutritional protocol that is served during in-patients treatment that’s actually going to promote a better composition of gut microbiota, increasing diversity which we know is associated with better health outcomes,” says West.
“If we can optimise this one small part then potentially we could see big implications down the line.”