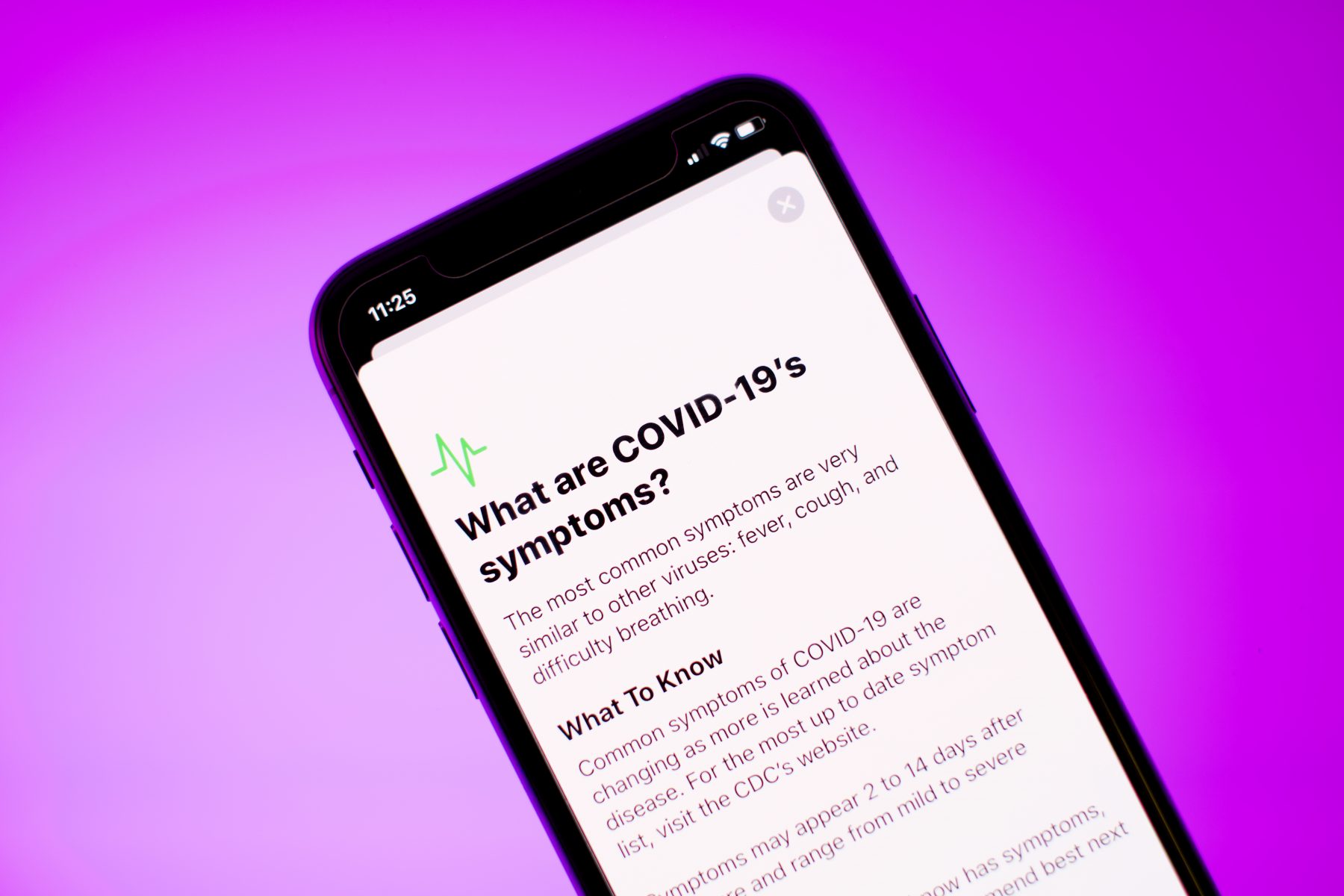
Telehealth has long been an underutilised service in Australia, but that could all change as our health systems adapt to the COVID-19 pandemic.
For Australians disadvantaged by distance or unable to easily leave the house, telehealth offers the chance to readily access health services by phone or video conferencing, particularly specialist health services that are hundreds or even thousands of kilometres away.
But until a few weeks ago, telehealth consultations were only covered by Medicare in a limited number of circumstances.
While many recognised the opportunity offered by widespread telehealth availability, it has been held back by traditional financing, regulatory and delivery models, along with the lack of standard technology across our health system.
That is now about to change.
Temporary Medicare and bulk billed cover
An expansion of telehealth in Australia in response to COVID-19 is underway. The federal government has announced a significant package for Australians to access healthcare via telehealth consultations.
After opening up a Medicare item for selected telehealth consultations for those requiring COVID-19 isolation in early March, the government is now offering rebates on a much wider range of telehealth consultations.
These positive changes introduce a temporary Medicare item to provide bulk billed coverage by health professionals who choose to offer telehealth for general practice, psychology and psychiatry, nursing, midwifery and selected allied health consultations.
The new arrangements will protect both patients and health professionals from the risk of infection while still allowing essential health care and scripts to be delivered.
Some face to face consultations will still need to go ahead but these virtual consults will be critical if we are to avoid an increase in health issues down the track due to delayed diagnosis and treatment, and to avoid a surge in mental health illnesses.
Virtual hospitals and video consultations
At the same time we are seeing some providers experiment with new service models, such as a virtual hospital for COVID-19 patients, along with expansion of essential services such as the extra $74 million for mental health services.
Video-conferencing is now freely available through many apps and web-based services for patients who have a mobile phone or computer connected to the internet, and the confidence and skills to use it.
Through these “tele” consultations, a patient can dial in to speak to their doctor or interact with them through their phone or computer screen from the comfort and convenience of their home.
The path to better healthcare
Countries such as Denmark have been building their national telehealth strategies in recognition of the key role telehealth will play in efficient, integrated person-centred health care.
As the Danish white paper makes clear, the shift to telehealth requires not just technology but also organisational and systemic change.
The urgent need to shift to remote health solutions as a result of COVID-19 may be the release valve we need to comprehensively shift to telehealth and remote health as integrated components of a more innovative and robust future health system in Australia.

To ensure a successful, permanent shift, we need to integrate these new solutions as much as possible into existing infrastructure and payment mechanisms – no easy task – and gather the intelligence on what works best as we roll these solutions out.
Working well includes positive health outcomes, positive patient experience and positive health professional wellbeing. We must also actively monitor the impact on health inequalities and health professionals themselves.
We should not be tempted to return to business as usual once the COVID-19 threat eases. What is now a temporary Medicare item needs to evolve into a permanent, integrated solution.
Anna Peeters is Director of Deakin University’s Institute for Health Transformation and a Professor of Epidemiology and Equity in Public Health.